When it comes to liver health, detoxification doesn’t always get the attention it deserves. Yet, with the rising number of fatty liver disease diagnoses, understanding how the liver detoxifies the body is more important than ever.
A healthy liver is lean and efficient, managing blood glucose, amino acids, and hundreds of other vital processes. None of these tasks are possible if the liver isn’t able to detoxify harmful substances effectively. However, there’s a lot of confusion about what detoxification really is and whether we can enhance this critical process.
In this article, we’ll explore the fascinating details of detoxification, clarify common misconceptions, and provide insight into how to best support this essential liver function.
What are toxins?
The medical definition of toxin is any substance created by microorganisms, plants or animals that is harmful to humans. A toxicant, on the other hand, is any poisonous substance that is produced by or is a by-product of human activity.
For simplicity, this article uses “toxins” as a general term for both, as their effects on the body are similar: they can harm organs, disrupt body systems, and impair overall health.
Endogenous toxins are made by the body as part of daily life. Exogenous toxins enter from external sources like air pollution, food additives, contaminated water, medications, and personal care products.
Toxins can damage vital organs like the liver and kidneys, impair the immune and reproductive systems, and even lead to chronic conditions such as cancer, stroke, or neurological diseases. Emotional stress and toxic relationships can also be considered “toxins,” as they negatively impact physical and mental health.
Who is affected by toxins?
We’re all exposed to toxins daily, but the extent varies depending on factors like diet, lifestyle, and environment.
That said, some people are more sensitive to toxins than others, including:
- Genetically predisposed individuals who have a reduced ability to metabolize toxins.
- Those with overactive immune systems, which can trigger inflammation in response to toxins.
- People with acute or chronic illnesses that lower their tolerance to toxic substances.
- Individuals with toxin-induced loss of tolerance, meaning their toxin “cup” is full and their body can tolerate no more.
As well, children are more vulnerable than adults to toxins because:
- Their still growing bodies are not as efficient at eliminating toxins,
- They absorb greater amounts of some toxins, and
- Each absorbed toxin is at a higher concentration due to their smaller size.
What is detoxification?
Detoxification is far more complex than simply “flushing out toxins.” It’s a sophisticated, multi-step process that transforms harmful substances into non-toxic, water-soluble compounds, which are then excreted through breath, sweat, urine, or feces.
While all cells contribute to detoxification to some extent, the liver is the powerhouse of this process, with secondary roles played by the gastrointestinal (GI) tract, lungs, kidneys, and even the brain.
How does detoxification work?
The body detoxifies in four stages, each requiring specific nutrients and enzymes.
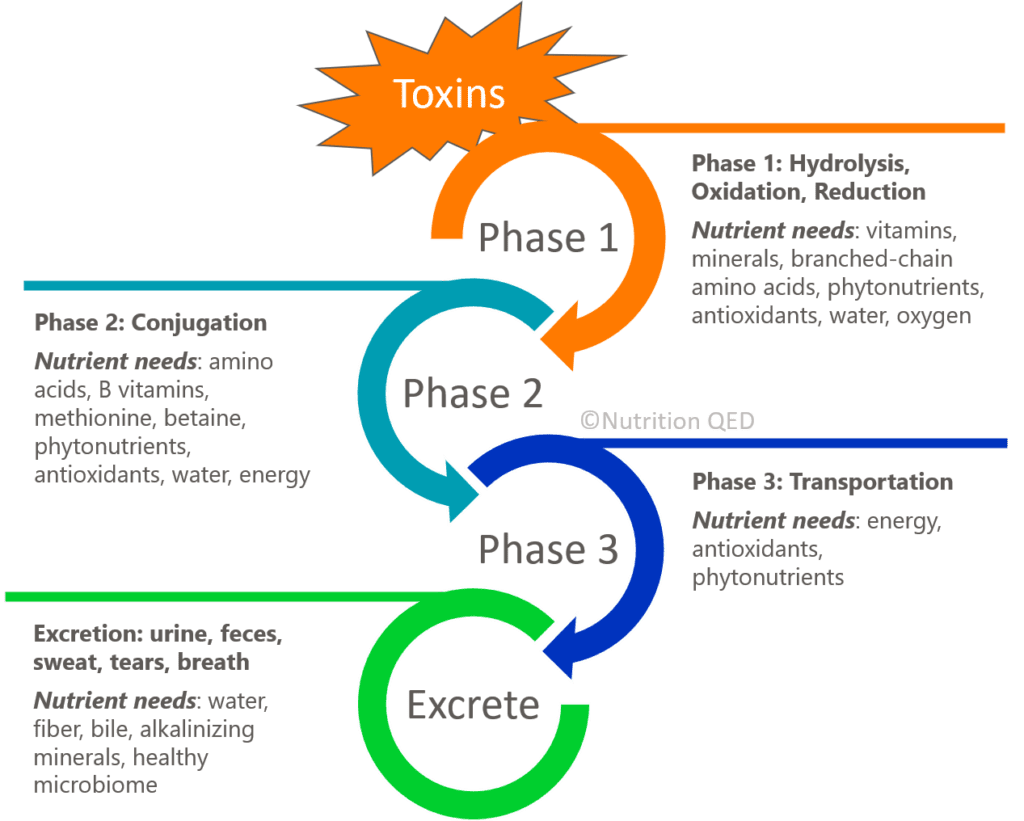
Phase 1: Hydrolysis, Oxidation and Reduction
Most toxins are fat-soluble, which allows them to dissolve and mix easily with fats. While this property helps them penetrate cell membranes, it also makes them incompatible with the body’s water-based fluids, such as blood and urine. To eliminate these substances, the body must convert them into water-soluble compounds that can be excreted.
Phase 1 detoxification begins this transformation process through chemical reactions such as hydrolysis, oxidation, and reduction. A diverse group of enzymes facilitates these reactions, including the cytochrome P450 (CYP) family, flavin-containing monooxygenases (FMO), and alcohol dehydrogenase. These enzymes work by chemically modifying toxins to make them more reactive and, ultimately, ready for the next phase of detoxification.
During this “bioactivation” stage, the metabolic breakdown often generates reactive oxygen species (ROS), commonly known as free radicals. While ROS are a natural byproduct of metabolism, they can be highly damaging to proteins, lipids, and DNA if left unchecked. Antioxidants, such as vitamins C and E, play a critical role in neutralizing these free radicals and preventing cellular damage. Without sufficient antioxidant capacity, the ROS generated in Phase 1 can cause oxidative stress and harm the body instead of aiding detoxification.
Although some toxins, like caffeine, can be fully metabolized and excreted during Phase 1, the majority require additional modification. These intermediate products are often more reactive—and sometimes more toxic—than the original substances, making Phase 2 detoxification essential for completing the process safely.
Key nutrients: Vitamins, minerals, branched-chain amino acids, phytonutrients, antioxidants, water, and oxygen are crucial for supporting the enzymatic reactions and antioxidant defenses in this phase.
Phase 2: Conjugation
In Phase 2 detoxification, the intermediate substances created during Phase 1 undergo further transformation to become non-toxic, water-soluble compounds that the body can safely eliminate. This phase, known as conjugation, involves attaching specific molecules to the reactive intermediates, effectively neutralizing their toxicity and enhancing their solubility for excretion.
A variety of enzyme families orchestrate Phase 2 detoxification. Key players include glutathione S-transferases (GST), which conjugate toxins with glutathione; N-acetyltransferases (NAT), which add acetyl groups; sulfotransferases (SULT), which transfer sulfate groups; and UDP-glucuronosyltransferases (UGT), which attach glucuronic acid. Each pathway targets specific types of toxins and requires a distinct set of nutrients and cofactors to function efficiently.
It’s important to note that the intermediate products formed during Phase 1 are often more reactive—and sometimes more harmful—than the original toxins. Without efficient Phase 2 detoxification, these intermediates can linger in the body and cause oxidative damage. This is why nutrient sufficiency and metabolic balance are critical.
For instance, the unpleasant symptoms of a hangover from excessive alcohol consumption can often be traced to a bottleneck in Phase 2 detoxification, no pun intended. The liver metabolizes alcohol into acetaldehyde, a toxic intermediate, during Phase 1. If Phase 2 detoxification (specifically the conjugation of acetaldehyde into acetic acid) cannot keep up, acetaldehyde builds up in the body, leading to nausea, headache, and other hangover symptoms.
Key nutrients: Amino acids, B vitamins, methionine, betaine, phytonutrients, antioxidants, water, and abundant energy (from carbohydrates, fats, or proteins) are essential for supporting the enzymatic processes of Phase 2.
Phase 3: Transportation
After toxins have been neutralized and converted into water-soluble compounds during Phases 1 and 2, the next step is transporting these compounds out of the cell. This critical process ensures the toxins can move through the body to their final destinations for excretion.
Specialized transport proteins embedded in cell membranes play the starring role in Phase 3. These proteins actively carry the detoxified substances across cellular boundaries. Depending on the compound, the transport proteins may move it out of the cell where detoxification occurred or into another cell for elimination.
This phase is highly energy-dependent, as the proteins require cellular energy in the form of ATP to perform their task. Additionally, some transport proteins rely on antioxidants and phytonutrients to maintain their structure and function, ensuring the safe and efficient movement of these compounds.
Key nutrients: ATP (energy), antioxidants, and phytonutrients are required for transporting the transformed toxins to their exit point.
Excretion: urine, feces, sweat, tears, breath
Once detoxified compounds reach their final destinations—such as bile, urine, or other excretory pathways—they are packaged for elimination from the body. The organs of excretion, including the kidneys, liver, lungs, skin, and gastrointestinal (GI) tract, work in tandem to rid the body of these substances.
- Urine: Water-soluble compounds are filtered by the kidneys and excreted in urine. Adequate hydration is essential to ensure proper kidney function and regular urination.
- Feces: Fat-soluble compounds are incorporated into bile, which is released into the digestive tract and excreted in feces. A diet rich in fiber and a robust microbiome support healthy digestion and regular bowel movements, crucial for effective toxin elimination.
- Sweat: Sweating, whether through exercise or heat exposure, helps remove certain toxins through the skin.
- Tears and Breath: Small amounts of detoxified compounds can be eliminated through tears and exhalation. Deep, intentional breathing can enhance this process, while crying may provide a small but meaningful release.
For efficient excretion, the body requires more than just a functioning liver. Nutrients like fiber, water, and alkalinizing minerals (e.g., magnesium and potassium) support the final stages of detoxification. Beyond nutrition, lifestyle factors like regular physical activity, sufficient hydration, and stress management are essential for optimizing the body’s excretory functions.
Key nutrients and habits: Adequate hydration, fiber, alkalinizing minerals, regular exercise, efficient digestion, daily bowel movements, sweating, crying, and deep breathing.
What about detox diets?
From a functional medicine perspective, a detox diet focuses on supplying the nutrients needed to support the liver’s natural detoxification pathways while minimizing toxin exposure. When done correctly, a detox can enhance the body’s ability to eliminate harmful substances.
How do I detox my body?
Your body is naturally equipped to detoxify when provided with the necessary nutrients and conditions. While detailed guidance is beyond the scope of this article, future posts in this series will offer actionable tips to help you support your liver’s detoxification processes.
Conclusion: Empower your liver’s detox superpower
Detoxification is one of the liver’s most impressive feats, helping protect your body from the harmful effects of toxins. By understanding how this process works and making informed choices about nutrition and lifestyle, you can support your liver’s ability to keep you healthy.
Stay tuned for the next post in this liver series, where we’ll dive deeper into practical ways to optimize detoxification.
In the meantime, if you want a 1-on-1 discussion to help you support your detoxification pathways, book a consultation. Let’s work together to build a healthier, toxin-free you!
Image by Christel SAGNIEZ from Pixabay.
Sources:
Environmental toxins are everywhere in our environment. (n.d.). How Environmental Toxins Can Affect Your Health. https://www.augusta.edu/online/blog/environmental-toxins
Integrative and Functional Nutrition Academy. Detoxification. Track 2, Module 6 [Handout].
Li, T., An, J., Xu, J., & Tuo, B. (2019). Overview of organic anion transporters and organic anion transporter polypeptides and their roles in the liver. World Journal of Clinical Cases, 7(23), 3915–3933. https://doi.org/10.12998/wjcc.v7.i23.3915
Li, Y., Yuan, H., Yang, K., Xu, W., Tang, W., & Li, X. (2010). The structure and functions of P-Glycoprotein. Current Medicinal Chemistry, 17(8), 786–800. https://doi.org/10.2174/092986710790514507
Metagenics Institute. (2018). The Role of Detoxification in the Maintenance of Health. In https://www.metagenicsinstitute.com. Retrieved December 4, 2024, from https://www.metagenicsinstitute.com/wp-content/uploads/2018/07/MET2221-Detoxification-Research-Review_MI.pdf
Morsy, L., & Rothstein, R. (2019, May 1). Toxic stress and children’s outcomes: African American children growing up poor are at greater risk of disrupted physiological functioning and depressed academic achievement. https://eric.ed.gov/?id=ED598149
Suls, J. (2017). Toxic affect: Are anger, anxiety, and depression independent risk factors for cardiovascular disease? Emotion Review, 10(1), 6–17. https://doi.org/10.1177/1754073917692863
Toxins: MedlinePlus Medical Encyclopedia. (n.d.). https://medlineplus.gov/ency/article/002331.htm
What you know can help You – An introduction to toxic substances. (n.d.). https://www.health.ny.gov/environmental/chemicals/toxic_substances.htm
Xu, C., Li, C. Y., & Kong, A. T. (2005). Induction of phase I, II and III drug metabolism/transport by xenobiotics. Archives of Pharmacal Research, 28(3), 249–268. https://doi.org/10.1007/bf02977789




